It is not uncommon for students with long-term health conditions to attend Drop-in to talk about their struggles with fatigue while studying. There are many conditions associated with fatigue. In Drop-in we would also see students going through the process of trying to get a diagnosis for a collection of symptoms; which presents its own wellbeing challenges. Common queries in the last year have featured Post-Viral Fatigue, Long Covid and Chronic Fatigue Syndrome.
Usually blogs are written on behalf of the Drop-in team. This one however, is personal to me, Drop-in Co-ordinator.
Recently, a student sought help to consider the option of deferring for a year while going through assessment for Chronic Fatigue Syndrome. She was concerned about the impact of her symptoms on her studies. When I shared my own experience of this situation, the student sent me a set of questions. She told me that the answers were very helpful to her. I thought that other students might feel the same way and have decided to share my experience, as I was diagnosed with Chronic Fatigue Syndrome whilst at university and opted to defer for a year. Here are her questions and my answers.
What helped most with your CFS?
- Diet: I used to rely a lot on sugar and caffeine to get me through periods of low energy but this led to severe sugar crashes and a vicious circle. I requested to speak to a Dietician who worked with me on snack planning of slow-release carbohydrates.
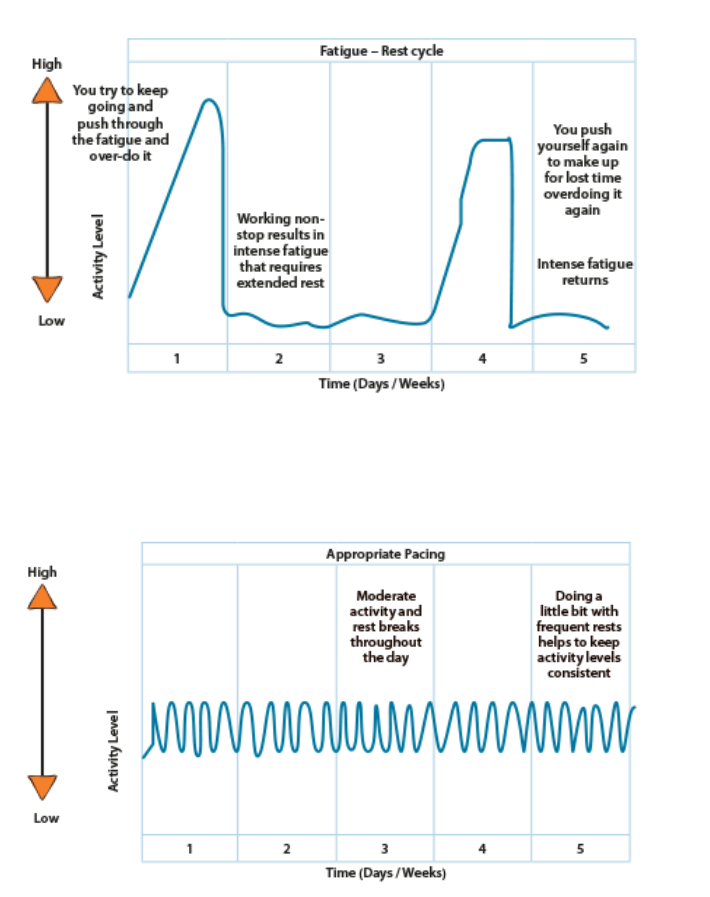
- Graded activity and planning: At first I used the ‘push through’ method which led to disappointment and further fatigue. Once I accepted that I did not have the same resources as my peers, I planned for rest and limited my activity, gradually increasing it over the years.
How did you find going back to studying after a year out?
It was tough. It was my final year so all my friends had graduated and I was with a new cohort of students. I was also not recovered. I managed by:
- Planning time around studies, rest breaks and being occupied at the weekends.
- Reminders that this was the final stretch and the discomfort was temporary to meet a goal.
What was your experience like getting diagnosed with CFS?
This involved about 5 years of investigations before a diagnosis was given. Different health trusts had different treatment options and there were waiting lists involved. In the end, it was self-directed research and self-management that led to improvements in symptoms.
What additional support did you get when you came back to Uni?
- Disability Services at my university to get extra time on exams in case it was needed needed.
- Disabled Students Allowance for recording equipment. This allowed me to record notes and listen back to them when my eyes were too tired to read. I put my headphones on every night to listen to my module content when going to sleep. I was offered other options such as a scribe in my exams.
- I created colourful mind maps of module content and posted them over my walls to help with memory.
What did you find helped?
- Rest- taking time to recharge after being overstimulated.
- Setting manageable goals that felt good to achieve.
- Massages and heat for physical pain.
- Changing diet.
- Gradual exercise.
- Setting boundaries. This involved learning to tell people no without feeling guilty.
- Reminders that this all takes time!
Any additional things that you think would help?
The answers to these questions are personal and specific to my situation. It is important to find what works for you. This could involve looking at daily routine, diet, exercise and the related thoughts and expectations of yourself. The ‘thought’ bit is very important. If you set a manageable routine but it brings you disappointment because you believe that you should be doing more, it will be less effective. The corresponding emotions to your actions take energy as well- such as anger, disappointment, etc. Therefore learning self-compassion is very helpful.
If you would like to talk to someone about the impact of fatigue on your wellbeing or studies, you can reach out for support at our Drop-in. If this is part of a long-term condition, you may wish to engage with Accessible Learning Support. If you are experiencing ongoing fatigue and are unsure as to the source of it, consider speaking to your GP.
Resources:
Lift Up Your Everyday – Managing energy – RCOT
How to manage fatigue – Muscular Dystrophy UK– image above credited to this site.
Royal College of Occupational Therapists- http://go.qub.ac.uk/managingenergy
Self Compassion: Self-Compassion | Action for Happiness
Bend Don’t Break Resilience Low Intensity CBT Workbook Ed Sipler – Bend Don_t Break.pdf (hscni.net)
